Book
Excerpts
Diabetic
Eye Disease:
Lessons From A Diabetic Eye Doctor
(How To
Avoid Blindness and Get Great Eye Care)
from Chapter
1: Lessons From A Diabetic Eye Doctor
What is "Good" Diabetes
Management?
Good diabetes management covers the span
of an individual's diabetic life (from the time of diagnosis forward)
but consists of a series of management decisions, treatments and
goals that change as a person's body changes (both due to the
normal aging process and the development of complications), as
new treatments become available, and as new strategies for improved
control are learned. This point cannot be stressed enough.
Like most chronic health conditions, there is no 'magic bullet'
for diabetes control. No "system" works perfectly forever,
and strategies must often change to keep up with changes in one's
health status. With advances in medical knowledge and biotechnology,
the "gold standards" of today will undoubtedly become
antiquated and sub-standard in the future. The history of medical
science is filled with examples of this phenomenon.
What does "good diabetes management"
mean? Foregoing medical jargon for now, a reasonable definition
might be: "controlling diabetes in such a way that the person
in question is able to experience life in the fullest way possible
without insurmountable physical disability caused by diabetes
and with a minimum of emotional stress." Put more simply,
good diabetes management means a patient suffers the dreaded complications
of diabetes to the smallest degree possible with the least hassle
possible. It does not necessarily mean patients will have no complications
(although that is certainly a worthy goal), only that those complications,
if they occur, will not prevent patients from reaching their life
goals or maximizing their unique human abilities.
Controlling diabetes effectively is an individualized
effort, but it should not be an individual one. Controlling diabetes
should be a team effort amongst the patient, her or his family
and closest friends, and a team of health care professionals who
are knowledgeable about and keenly interested in diabetes. I am
intimately familiar with several different strategies for controlling
diabetes, both as a Type 1 diabetic for 34 years, and as a doctor
of optometry managing the eye complications of diabetes for the
last 12 years.
I have managed my own condition differently
at different points in my life, and I have seen several thousand
of my own diabetic patients manage their conditions using a variety
of different strategies. Some diabetics ignore their disease,
living life exactly as they did prior to diagnosis. Others meticulously
monitor their blood sugars, medications and diets, frequently
consult with health care professionals to check for the earliest
signs of diabetes complications, read many journal articles describing
all the latest diabetes research, and attend lectures on every
aspect of diabetes management. Most diabetics probably fall somewhere
between these two extremes. Somewhere in between is where I started
34 years ago...
...The evolution of my strategies for managing
my diabetes has not been easy, and there have been many setbacks
along the way. I still have some high blood glucose readings due
to over-indulgence, forgetfulness, illnesses like the occasional
cold or flu, poor planning, stress and the vagaries of human existence.
I very nearly lost my eyesight and was heading toward kidney failure,
so my lifelong diabetes management strategy certainly has been
no paragon of virtue. Of course, I will have to continue managing
my diabetes for the rest of my life, or until a definitive cure
is found...
from Introduction to Section II -
Diabetic Eye Disease
In this section, we will consider in some
detail the several different forms of "diabetic eye Disease,"
building upon the fundamentals discussed in previous chapters
and stressing the steps every diabetic can and should take to
reduce the risk of eye complications. Importantly, many of these
risk reduction strategies will have the added benefit of reducing
the risk of all diabetes complications, both microvascular (eyes,
kidneys and nerves) and macrovascular (heart, brain and large
blood vessels).
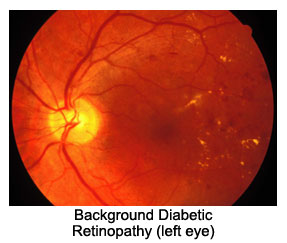
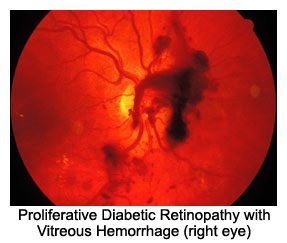
When thinking about the eye complications
of diabetes, most people, including most health care professionals,
think of diabetic retinopathy, the process through which the eye's
light sensitive retina is damaged by chronic hyperglycemia. Indeed,
diabetic retinopathy is arguably the most important example of
diabetic eye disease, as it accounts for more than 22,000 cases
of legal blindness each year in the United States, and more than
200,000 cases annually Worldwide. However, diabetic retinopathy,
which has several different forms and stages, is itself only one
of several completely distinct types of "diabetic eye disease."
Recognition and understanding of each of these particular types
will help health care providers and patients alike to recognize
specific eye and/or vision symptoms related to previously diagnosed
diabetes and, perhaps, to suspect undetected cases of diabetes
when a clinical diagnosis has yet to be made.
There are seven different "diabetic
eye diseases": diabetic cataract; glaucoma; diabetic keratopathy;
diabetic optic neuropathy; diabetic cranial neuropathy; diabetic
retinopathy; and retinal vascular occlusion. Each affects a different
part of the eye, from the nerves that control eye movement to
the nerve that connects the eye to the brain, from the front surface
of the eye to its innermost internal layers. To better appreciate
these various diseases, it will be helpful to conduct a "crash
course" of sorts in ocular (eye) anatomy.
From there, we will explain the various
kinds of diabetic eye disease, the treatments available for each
and the things you can do to prevent or minimize vision loss from
diabetes. Finally, we will consider the necessary elements of
a thorough diabetic eye examination, including questions to ask
your eye doctor and questions she should ask you, as well as some
very important information about what to do if and when diabetic
eye disease causes significant visual impairment.
It is extremely important that all diabetics
understand a fundamental distinction between good eyesight and
good eye health. The ability to see clearly (on an eye chart test
or in the real world) is not equivalent to having healthy
eyes. Many patients with serious eye disease have excellent eyesight,
and the vast majority of patients who require eyeglasses or contact
lenses to see clearly have healthy eyes. Just as for many patients
with heart disease or cancer, patients with eye disease often
have no symptoms until it is "too late." Regular, comprehensive
eye examinations by an eye care professional (optometrist or ophthalmologist)
are the best way to ensure both good eyesight and good eye health.
from Chapter 11 - Diabetic Retinopathy
Diabetic retinopathy is perhaps the single
most important cause of adult blindness in the Western World,
and almost 15% of all blindness in the United States is caused
by diabetic retinopathy. This statistic takes on added economic
significance when we consider the fact that many of these cases
occur in younger adults who are often in the prime of their income
earning years.
Diabetic retinopathy, unfortunately, is
a very insidious disease. It usually causes no symptoms in its
earliest, most treatable stages, and by the time symptoms are
noticed, many patients have experienced irreparable damage and/or
loss of vision, and the overall prognosis is poorer. This is why
dilated eye examinations by an experienced and knowledgeable eye
doctor are so vital. The earlier retinopathy is detected, the
more can be done to prevent, or at least delay, significant loss
of vision.
The retina lines the inside surface of the
eye, like wallpaper covering a wall. It has seven distinct layers,
each with unique characteristics and functions, which are readily
observable under a microscope. In the clinical setting (i.e. the
eye doctor's office), the individual layers are not all directly
observable, but a variety of examination tools and techniques,
combined with intimate knowledge of retinal anatomy, allows the
eye doctor to examine the layers damaged by diabetes, to make
a diagnosis and evaluate the type and severity of diabetic retinopathy,
and to make treatment recommendations. Such recommendations may
include observation over time, improved blood sugar control, laser
treatment of the retina, use of prescription medications, surgical
treatment of the retina, or a combination of these.
The Normal Retina
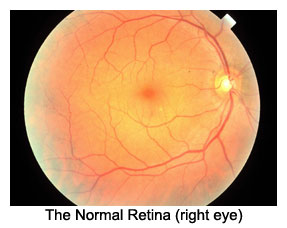 The
normal retina contains many blood vessels. Large arteries coming
from the neck (the carotid arteries) branch off into smaller arteries
serving the eye (the ophthalmic and ciliary arteries) which branch
off into smaller arterioles coursing through and beneath the retina
(retinal and uveal arteries, respectively) which branch off into
thousands of microscopic capillaries designed to deliver blood
to each bit of retinal tissue.
The
normal retina contains many blood vessels. Large arteries coming
from the neck (the carotid arteries) branch off into smaller arteries
serving the eye (the ophthalmic and ciliary arteries) which branch
off into smaller arterioles coursing through and beneath the retina
(retinal and uveal arteries, respectively) which branch off into
thousands of microscopic capillaries designed to deliver blood
to each bit of retinal tissue.
Diabetic retinopathy alters this normal
anatomy and its function in several distinct steps or 'stages,'
each of which has its own characteristics. The 'earlier' stages
are less worrisome, but may progress to the vision-threatening,
advanced stages unless something intervenes (whether that 'something'
is better blood sugar control, blood pressure control, laser treatment,
luck, or some other factors that have yet to be fully understood.)
Here, we will consider the stages of retinopathy...
...Research has clearly shown that intensive
diabetes management, including lowering blood glucose and blood
pressure levels, greatly reduces the risk of getting diabetic
retinopathy, and slows down its progression (worsening) in patients
who do have it. In fact, the DCCT showed that a 10% reduction
in HbA1c reduces the risk of retinopathy progression by 43%, while
the UKPDS showed that better control of blood pressure reduced
the risk of worsening retinopathy by up to 34%.
Many experts believe that retinal capillaries
are damaged when blood glucose levels approach 180 mg/dl on a
consistent basis (this is equivalent to a HbA1c of 8.0%.) This
is why most guidelines recommend that patients strive to keep
their average blood glucose at or under 150 mg/dl (equivalent
to an HbA1c of 7.0% or less.) To achieve these targets, patients
should perform regular home blood glucose tests and adjust their
diet, exercise and medications accordingly. They should also work
closely with their doctor to find the right medications and dosages,
perform quarterly glycosylated hemoglobin tests, and monitor their
blood pressure and blood lipids.
After having diabetes for 10 years, 60%
of patients will have at least the beginning stages of retinopathy;
after 20 years, that number jumps to more than 90%. This underscores
the general rule that the longer a person has diabetes, the greater
is the chance of having complications. The best way to detect
diabetic retinopathy is through regular dilated retinal exams,
the importance of which cannot be over-emphasized in early treatment
and prevention of vision loss.
from Chapter 15 - Low Vision
Knowledge is Power, and a form of
Cheap Insurance
Unfortunately, many people have already
suffered the eye complications of diabetes. More tragically, many
people will continue to suffer vision loss in spite of all we
know, and the good news about prevention and effective treatments.
Hopefully, far fewer diabetics will experience complications in
the future. Hopefully, a definitive cure for diabetes is just
'around the bend.'
Until that time, though, it is very important
that all diabetics know about what can be done, right now, to
help them cope with vision loss. For those who have already experienced
vision loss, this chapter may serve as a primer on what's available
and how to get started. For those who haven't lost vision from
diabetes, the information in this chapter might best be viewed
as an 'insurance policy' of sorts; Hopefully, it will never be
needed, but it will be nice to have some familiarity with this
material, "just in case."
Click HERE
to return to Book Information.
Copyright 2006 by DiabeticEyes.com
~ All Rights Reserved
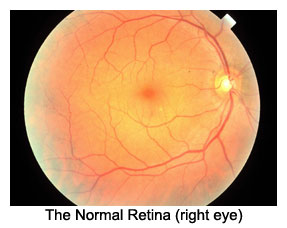 The
normal retina contains many blood vessels. Large arteries coming
from the neck (the carotid arteries) branch off into smaller arteries
serving the eye (the ophthalmic and ciliary arteries) which branch
off into smaller arterioles coursing through and beneath the retina
(retinal and uveal arteries, respectively) which branch off into
thousands of microscopic capillaries designed to deliver blood
to each bit of retinal tissue.
The
normal retina contains many blood vessels. Large arteries coming
from the neck (the carotid arteries) branch off into smaller arteries
serving the eye (the ophthalmic and ciliary arteries) which branch
off into smaller arterioles coursing through and beneath the retina
(retinal and uveal arteries, respectively) which branch off into
thousands of microscopic capillaries designed to deliver blood
to each bit of retinal tissue.